Mosquito-borne disease in New Zealand
How Aotearoa New Zealand's health has been affected by mosquito-borne diseases which cross our international borders.
On this page:
Mosquito-borne disease notification counts have increased since 2005, particularly from 2014
Five mosquito-borne diseases were detected in New Zealand in 2019 [1]:
- Four mosquito-borne viruses: Chikungunya, Dengue Fever, Ross River Virus and Zika
- One mosquito-borne parasitic disease: Malaria
Mosquito-borne disease notification counts have increased from a low in 2005, with peaks occurring in 2014, 16 and 18 (Figure 1). This trend was driven by an increase in the number of Dengue cases and the emergence of Zika and Chikungunya since 2014.
Figure 1: Number of case notifications of mosquito-borne diseases in New Zealand, 2001-2019
Source: Episurv, ESR 2020
Differences in the characteristics of people who had mosquito-borne diseases
Among people diagnosed with mosquito-borne diseases in New Zealand, there were:
1. Differences in overseas travel
The Pacific was the most frequently visited region among people returning with Dengue and Zika from 2018–19. Asia was the most frequently visited region for people returning with Chikungunya while Africa was most visited by those returning with Malaria [2, 3].
All individuals diagnosed with mosquito-borne diseases in New Zealand, in 2018 and 2019, were thought to have acquired these diseases while travelling overseas [2, 3]. However, there were cases classified as "unknown".
2. Differences in age:
Over the three-year period, 2017–19, mosquito-borne disease notification rates were highest in individuals aged 25–44. Children (0–14 years) and individuals aged 75+ years had the lowest notification rates [1]. These low rates may partially reflect the frequency of international travel by age. New Zealanders aged 0–14 and 75+ years make up 34% of the population, while only 16% of returning travellers fall into these age groups.
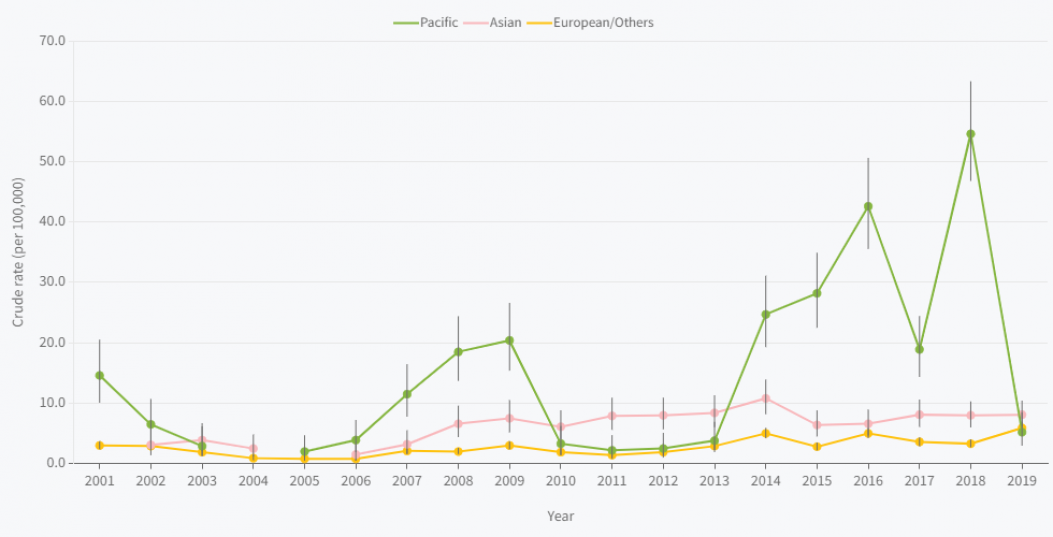
3. Differences in ethnicity:
Since 2001, Pacific Peoples have commonly had the highest rates of mosquito-borne disease in New Zealand. In 2018 cases of mosquito-borne disease among Pacific peoples reached their highest rate (54.6 per 100,000) since 2001, roughly 17 times greater than the European/Other ethnic group rate (3.2 per 100,000) [1]. However, in 2019 rates among Pacific Peoples dropped to 5.2 per 100,000, due to a drastic decrease in Dengue cases.
Figure 2: Mosquito-borne disease notification rates, New Zealand, by prioritised ethnicity, 2001-2019
4. Socio-economic differences in rates of mosquito-borne disease:
For the 2015–18 period, there were differences in the notification rate of mosquito-borne disease by level of socio-economic deprivation. More deprived areas, quintiles 4 and 5, regularly had higher rates than less deprived areas, quintiles 1 and 2 [4]. However, in 2019 this trend reversed with infection rates in the most deprived quintile (3.5 per 100,000) being less than half the rate recorded in the least deprived quintile (8.1 per 100,000).
5. Differences by region:
Over the period 2017–19, the rates of mosquito-borne disease in the Auckland (11.3 per 100,000) and Counties Manukau (9.7 per 100,000) District Health Boards were approximately twice the national rate (5.8 per 100,000) (Figure 1) [1].
References
1. Institute of Environmental Science and Research Limited (ESR). Notifiable diseases EpiSurv data extraction. Porirua: Institute of Environmental Science and Research Limited. [2020 personal communication with ESR Senior Analysts]
2. ESR. 2020. Notifiable Diseases in New Zealand: Annual Report 2018. Porirua: Institute of Environmental Science and Research Limited. URL: https://surv.esr.cri.nz/PDF_surveillance/AnnualRpt/AnnualSurv/2018/2018AnnualNDReport_FINAL.pdf (accessed 12 August 2021).
3. ESR. 2021. Notifiable Diseases in New Zealand: Annual Report 2019. Porirua: Institute of Environmental Science and Research Limited. URL: https://surv.esr.cri.nz/PDF_surveillance/AnnualRpt/AnnualSurv/2019/2019AnnualNDReport_FINAL.pdf (accessed 12 August 2021).
4. Atkinson J, Salmond C and Crampton P. 2014. NZDep2013 Index of Deprivation. Wellington: University of Otago
